Cardiopulmonary Development
Studying how the heart and lungs develop before birth
Background image: Branching tips and airways in human lung tissue at 10 weeks of development (Image by John Russell, Rawlins lab)
After birth, the heart and lungs work together to supply oxygenated blood to the whole body.
In the embryo during pregnancy, the two organs develop closely together and must both be fully-functional by birth for the baby to survive outside the mother.
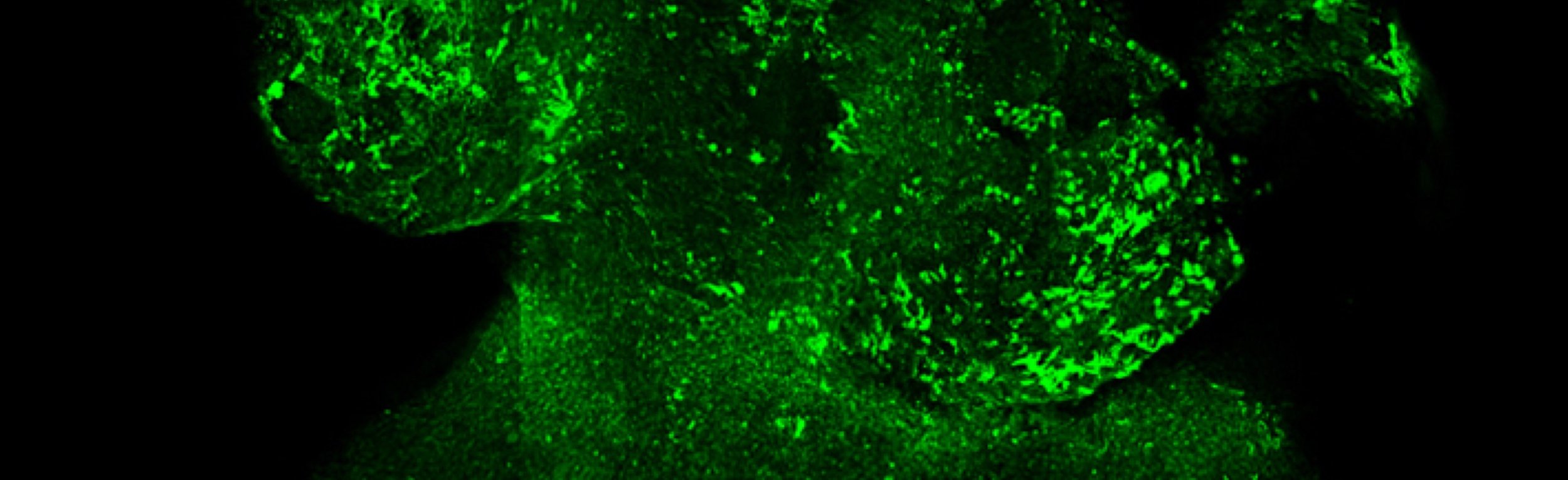
The heart forms as a tube that is later divided into sections, forming the chambers of the heart. Defects in this separation account for most cases of congenital heart disease. Meanwhile, the surface of the lungs which enables oxygen to enter the blood (the gas exchange region) must be formed by the end of pregnancy in order for the baby to survive outside the womb. We are studying how the separating walls in the forming heart are made, which cells contribute to their formation and how different lung stem cells work together to build the gas exchange region of the lungs.
Cells cultured from human lung tissue at 10 weeks of development (Image by John Russell, Rawlins lab)
The cardiopulmonary system functions as a unit in the adult and develops together in the embryo.
Background image: Outer layer of the human heart at 41 days of development (Image from the Riley lab)
Cells from the outer layer of the human heart at 41 days of development (Image from the Riley lab)
Cell lineage and spatial patterns of morphogenesis are strongly linked across the developing heart and lungs. Septal and gas exchange surface defects in the heart and lung respectively contribute to congenital disease, mortality and morbidity in premature neonates.
We are using clonal analyses to study heart septation and lung gas exchange surface development, providing a baseline for the analysis of cardio-pulmonary disease. We are also testing the hypothesis that multipotent mesenchymal progenitor populations contribute to the entire cardio-pulmonary system during fetal stages, as has been suggested by studies in animal models. To address these, we are developing organ culture and imaging technologies that could be more broadly applied to human organogenesis.

Members
-

Prof Emma Rawlins
Gurdon Institute, University of Cambridge
We study the roles of stem cell populations in lung development and repair aiming to understand how lung stem cells choose to make the different mature cell types that make up our lungs. We use complementary human organoid and animal models, molecular genetics and advanced microscopy to study this problem.
-

Prof Paul Riley
We study heart development and regeneration, focusing on the epicardium, lymphatics and the immune cells during heart formation and in response to injury (myocardial infarction or “heart attack”). We have a long-standing interest in cardiac morphogenesis, including septation (of the ventricle and great vessels), for which we employ state-of-the-art microscopy and animal models of congenital heart disease.
-

Prof Shankar Srinivas
We aim to understand how the heart forms and starts to beat. We focus specifically on the origin of the earliest cells that form the heart using multidisciplinary approaches including molecular genetics and live imaging.
-

Dr Sam Behjati
The Behjati lab works on the developmental origins of cancer, with particular focus on childhood cancer, combining cutting edge single cell transcriptomics and cancer genomics.
-
Dr Yang Li
(Rawlins lab)
-

Dr John Russell
(Rawlins lab)
-

Dr Claudio Cortés Rodríguez
(Riley lab)
-

Dr Matthew Stower
(Srinivas lab)
-
Former members
Dr Lucía Cabriales Torrijos
Dr Kevin Chalut
Dr Brittany Croft